Yalta in West Africa
Ebola’s presence is felt almost immediately upon landing in Conakry. On the way into the city from the airport, judiciously placed billboards dot the landscape, proudly affirming the Guinean government’s engagement in fighting the epidemic. In Conakry, as throughout West Africa, buckets of chlorinated water—or sometimes an alcohol–water solution—stand guard, their presence a constant injunction to disinfect one’s hands.

Figure 1. Pool of the Palm Camayenne, Conakry.
The exception to the rule is the Palm Camayenne hotel, located on Conakry’s corniche (Figures 1, 2). Here, there is no injunction to disinfection: guests can enter unhindered. The Palm Camayenne is one of the rare hotels in Conakry that offers western-style accommodations and 24 hours of electricity and Internet a day. As a result, it has become the home base for the delegations that have been marshalled in the response to the epidemic. Staff from the U.S. Centers for Disease Control (CDC), France’s medical research agency INSERM (Institut National de la Santé et de la Recherche Médicale), the Belgian Institute for Tropical Medicine, UNICEF, the World Health Organization (WHO), and many other global health agencies headquarter at the hotel. Ebola is the chief subject of discussion at the Palm Camayenne: the latest government measures, news from the myriad coordination meetings held during the day, epidemiological updates, or the preparation of clinical trials pepper conversations, whether over dinner, at the bar, or poolside.

Figure 2. Courtyard of the Palm Camayenne, Conakry.
The hotel even offers a special that includes room and board. Initially called the “Ebola pack,” the offer has since been rebranded the “NGO pack”: the initial appellation was perhaps subject to misinterpretation. The hotel takes pains to detail the security measures “both active and passive” to ensure against the epidemic, including “hazard analysis critical control point,” or HACCP, to ensure food hygiene, constituting a de facto microbiological bunker from which operations can be directed at minimal risk to foreign teams. Ebola too has its Yalta.

Figure 3.
The Baghdad Boys
In Guinea, as in elsewhere in Africa, youth gangs have become important political actors. Since the end of the régime of Lassana Conté, during the coup that brought the military junta to power, and during the recent elections, Guinean youth groups—going by the English appellation of Staff, or Gang, or in French, bande—have been at the forefront of popular discontent. Despite their association with violence and illicit activities, the youth gangs are nonetheless considered legitimate in their protest against predatory and extractive—in the case of Guinea’s mineral wealth—practices. When actors such as Médecins Sans Frontières (MSF; Doctors Without Borders) or the Red Cross intern patients in camps, “disappear” the bodies of the dead without families present, or bury them in unmarked graves, a powerful symbolic equivalence is established with state predation. It is perhaps not surprising that it is the youth gangs that have instigated at times violent resistance to Ebola efforts: not as a nihilistic gesture, but as a broader politics of rejection of the pillaging of the country by corrupt local and foreign elites.
As central actors of political life in Guinea, youth participate in preventive interventions: in Guéckédou (see Figures 4,5), the “Bagdad staff” organized an Ebola football competition. Whether to contest MSF actions or to foster prevention, youth occupy a place where authorities (elders, the state) are seen as illegitimate. It also signals the subterranean and chronic conflicts that pit generations against each other in a time of diminishing returns.
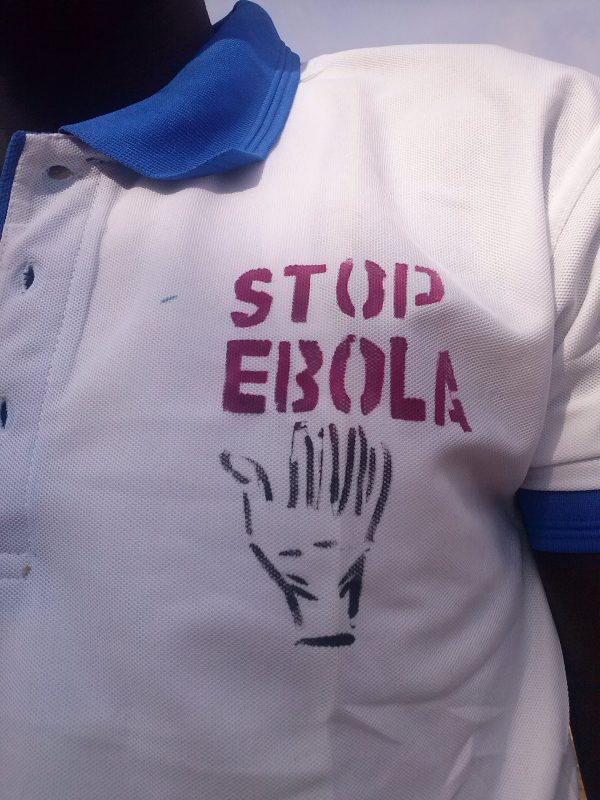
Figure 4. Baghdad Staff to Stop Ebola.
Ebola crystallizes pre-existing political tensions: between urban elites and rural populations, between elders and youth. Are those in charge of the epidemic there to protect, or just to pilfer the ostentatious display of resources mobilized against the epidemic?
This breakdown in trust, already endemic, has been dramatically heightened with Ebola: the media overload of images of foreign workers in isolation suits, sometimes chasing down escaped patients, saturates questions of social relations and intimacy with the fear of contagion. This epidemic is certainly a political crisis, but it is also a moral crisis.

Figure 5.
On Preparedness: Guinea as Laboratory

Figure 6. The anthropologist (FLM) prepares for fieldwork in an ETU.
The Ebola outbreak has put Guinea on the global health map. The engagement of diverse actors aiming at curing or finding proper treatment using gold standard biomedical knowledge production fosters both hope and competition between local actors.
Locals with medical or scientific training have seen the opportunity. One of them (I call him Abdul) takes me to visit his newly opened organization, which surfs on global health key words (sustainability, development, health). In fact, he wants to sell me a product: he is developing a clinic with a lab for running blood tests, and he wants to perform community health surveys. His project seems at first glance dubious, but when we get to his home, things become interesting. He has in fact transformed his domicile, in a well-heeled suburb of Conakry, into a laboratory. We visit the four floors of his house, which is something out of a survivalist manual. The house is off the grid, generating its own electricity with solar panels (with a generator and batteries for back-up) and is self-sufficient in water (well and tanks on the roof). There are a guest apartment, offices, a small canteen also on the roof, classrooms, a conference room with touchscreen, and a fully-equipped P2 lab easily turned into a P3: centrifuges, freezers, PCR booths, etc.
I (FLM) discussed the epidemic with Abdul. He doesn’t like the term “postcolonial,” although he concedes that one has to understand the “political influences.” I ask him why there is not yet a vaccine trial in Guinea. He retorts that France is not “doing its job” even though Guinea is its responsibility: the proof is that at a WHO vaccine meeting at the end of October, the United Kingdom and the United States sent their health ministers, whereas the French “only” sent their Ebola czar. It has become a common complaint that there is a kind of postcolonial struggle for Africa occurring because of Ebola, with the Americans setting up camp in Liberia, the British in Sierra Leone, and the French in Guinea. Abdul’s complaint is different: there needs to be more of a scramble and, in a knowing historical analysis, that postcolonial strings are the ones that need to be pulled for this to happen.
On Preparedness: Drills and Angst on Remote Front Lines

Figure 7. Boarding for Paris, Conakry Airport.
The emergency room where I (VKN) work is another kind of Ebola front line: Hospital A, the first major teaching hospital between Charles de Gaulle Airport and the city of Paris, lies amid a ring of cités (projects) that form a beltway of urban poverty around northeastern Paris. The vast majority of patients are migrants, many from West Africa. As a result, many who work there consider Hospital A the “front line” for the first domestic Ebola cases. However, preparedness for Ebola has focused on a larger Parisian hospital and a military hospital in the wealthier southern suburbs where all the expatriates with Ebola brought back to France have been treated—and cured. Preparedness in France rests on two fundamental assumptions: that Ebola patients can be screened prior to boarding flights to Paris (using pistol-like thermometers to take temperatures before boarding, as shown in Figure 7), and that potential cases that get through will be triaged over the phone by France’s unique emergency medicine system before they arrive at health care facilities.
At Hospital A, preparations for handling Ebola cases were slow to start, but gradually picked up steam around the same time that Thomas Eric Duncan was sent home with Ebola from Texas Presbyterian Health in Houston. Masks and personal protection gear showed up, and drills were conducted. But this kind of preparedness has an Achilles heel: the assumption that it is actually possible to reliably triage those who are stricken with Ebola from those who are not. Most of the health care workers infected with the virus in Africa were not working in specialized Ebola treatment units: they were exposed in the routine work in emergency departments, hospital wards, and maternity units. Patients with Ebola have the same symptoms as those with malaria, or typhoid, or any number of infectious diseases overwhelmingly prevalent in African health care settings, and common in the north. And it is simply not possible to work in those settings cloaked in the kind of personal protective equipment used in Ebola cases.
So might Parisian hospitals be preparing (Figure 8) for the wrong scenario? The current situation (where suspect cases are triaged to specialized hospitals) has put an enormous strain on the affected hospitals. Even though none of the suspected cases has been in fact confirmed, every case mobilizes staff, time, and resources as patients are transferred out of containment wards, clinical and lab staff suit up, and crisis management teams convene. In West Africa, health officials are paying more attention to the coming tsunami of deaths from malaria, childbirth, and other causes of mortality left untreated. But even on remote “front lines” such as in Paris, preparedness for the wrong epidemic may in fact be a distraction from more pressing and immediate health concerns.

Figure 8. Ebola preparedness drill in the Emergency Department.
