“The effects seen in in utero des-exposed humans parallel those found in contaminated wildlife and laboratory animals, suggesting that humans may be at risk to the same environmental hazards as wildlife.”
(Wingspread Declaration, 1991)
In April 1970, Arthur Herbst and Robert Scully reported in Cancer the identification of six definitive cases of cell vaginal cancer in girls and young women all between 15 and 22 years old. Continuing the investigation through a case-control study, the Herbst team published its findings in the New England Journal of Medicine:
This form of cancer was significantly associated with diethylstilbestrol (DES) use by the patients’ mothers during the first trimester of pregnancy.
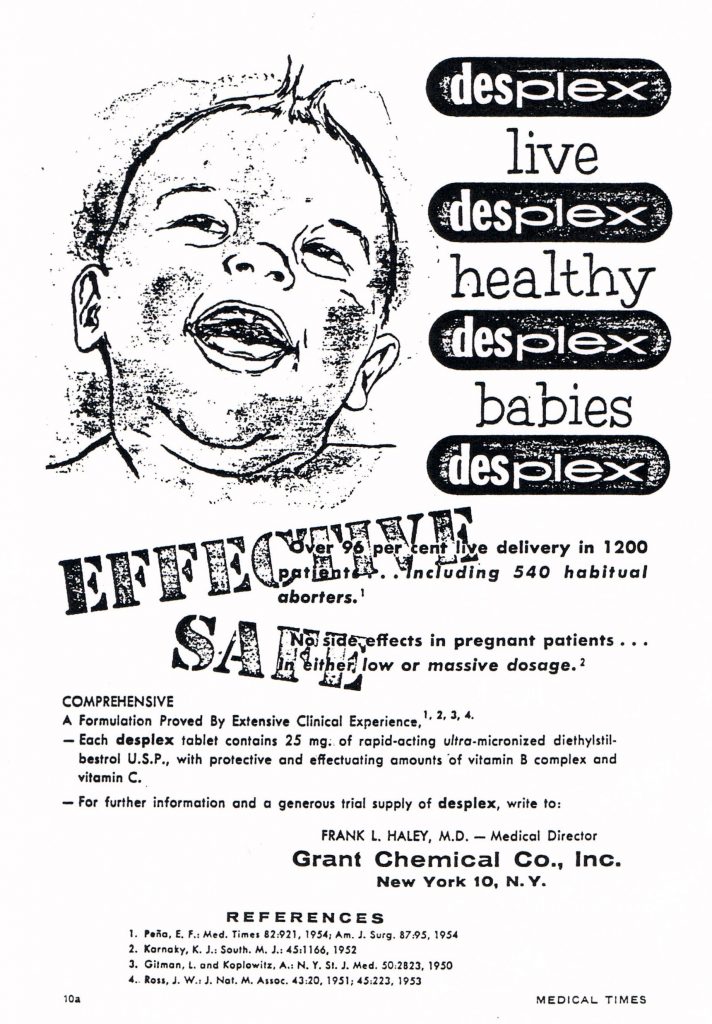
DES, a hormone synthesized by Doods in 1938 in England and approved by the FDS in 1941, had been widely prescribed by physicians to prevent miscarriages throughout the developed world in the following decades. Their study on DES effects was the first time a link was shown between taking a medicine during pregnancy and a subsequent morbid effect with considerable temporal distance on the offspring.
Since the early 1970s, the list of actual or potential effects of in utero DES exposure has grown steadily to include infertility, high prematurity, urogenital malformations, cancers, psychiatric disorders, eating disorders, congenital oesophagial stenosis, and other conditions. Populations found to be affected by exposure started with “DES daughters” but were later found to also include “DES sons” and “DES grandchildren.” A new category of disease thus appeared: transgenerational diseases.
In 1991, a group of scientists met at the initiative of Theo Colborn and Pete Myers, American researchers searching for links between environmental exposures and health. All of them were concerned about the effects of chemicals as a potential threat to reproduction of enormous scope. They stated that DES was the first endocrine disruptor identified. Accordingly, the lessons relating to DES should provide the necessary model to anticipate threats posed by other substances to animal and human development. However, the previous history of this molecule shows a complete lack of precaution about its side effects.
The disregard of repeated warnings marked the U.S. history of regulating DES from the first prescriptions in the 1940s until physicians were ordered to stop prescribing the drug to pregnant women in 1971 (Langston 2009). The French story goes beyond what happened in the U.S.: DES prescription began in the early 1950s and peaked in the late 1960s; it was recommended for use in pregnant women until 1976 and—unlike the case in the U.S.—continued to be used marginally until at least 1982. Our work on French DES raises the question of why scientific warnings about the dangerous effects of the drug did not have a “sentinel” effect. In the following pages, we will show different mechanisms of invisibility that prevented public knowledge and collective learning.
Considering pharmacovigilance about side effects of DES as a drug, we observe the repeated tragedy of institutional neglect leading to long-term health problems among DES progeny. Looking at DES with environmentalist glasses as a precursor substance of endocrine disruptors (ED), we see a wide mobilization and a pro-active vigilance: the studies of DES exposure along with observations of wildlife in polluted environments shaped the Wingspread Declaration in 1991 (Krimsky 2000). And twenty years after the declaration, DES is used routinely in animal experiments to measure the effects of other suspected endocrine disruptors.
In short, the DES story is that of a disastrous medical and social experiment that was later identified as having created valuable precedents helping to trigger the development of new tools to prevent similar damage (Chateauraynaud & Torny 2005). These two successive movements are typical “late lessons from early warnings” in which collective learning took place slowly in the USA, and even more so in France.
In North America, after the initial harms of DES were shown, the medical establishment in the 1970s quickly mobilized to mitigate damages and subsequently established follow-up cohorts to monitor health problems in DES offspring. DES victims mobilized later in the French case, and more than two decades separate the American and French DES tort law trials. The French history can therefore shed a different light on the legacy of DES: It poses the question of how knowledge about transgenerational diseases was not built on these sentinel populations. In other words, under what circumstances does an alert not lead to action?
A non-existent sentinel group: DES-exposed progeny
Understanding the non-existence of sentinel populations in the DES case first requires exploring prescription patterns in the 1950s and 1960s in France. In the absence of standardized guidelines and without any pharmacovigilance infrastructure, prescription requirements were highly variable. Herbst’s 1971 discovery was not widely disseminated in France because of weak links between French obstetricians and the American epidemiological universe. When Herbst spoke at a conference in Paris in 1972, most obstetrician-gynecologists did not believe in the risk of cancer caused by DES for their patients. The doubts of this audience were in part due to differences in principle—the hormonal theory of miscarriages still masked the genetic theory—and, more pragmatically, due to the claim made by many French doctors that DES was prescribed in far lower doses in their country. Only a handful of clinicians “recalled” their patients so they could inform their daughters. Most notable among this group was Dr. Jeanine Henry-Suchet, who attempted to mobilize her colleagues to act, but did not succeed. As a result, in the 1970s, most girls exposed in utero were unaware of their exposure and its attendant risks. Even when the contraindication of DES for pregnant women was adopted in 1977, there were no traces of a public discussion.
Worried by new results concerning fertility problems suffered by “DES daughters” and by some uterine malformations in her patients, Dr. Anne Cabau searched for DES daughters through the magazine of a mutual benefit society in 1981 and published some clinical results. Following Cabau’s piece, le Monde published an article titled “A Monumental Mistake” in 1983, which was widely quoted by mainstream media. Most public health institutions took reassuring stances, stating that the problem was already widely known and mostly a matter of the past. A group of scientists mobilized by the “French NIH” (INSERM) issued recommendations outlining how to support and inform patients. But these recommendations remained a dead letter despite the scientists’ conclusion that 160,000 children had been exposed in utero to the drug.
In 1988, following the advocacy of a patient’s association, a group of clinicians and researchers met at the Ministry of Health to develop a brochure about the dangers of DES. The vast majority of these experts rejected distributing the brochure to patients, arguing it should only target health care professionals. As a result of doctors’ resistance to broader outreach and education, the effect of this initial campaign was very limited. A second campaign was launched in 1992, and in 2003 AFSSAPS, the “French FDA” did it again. But the level of knowledge among gynecologists stayed very low as they felt they were not concerned.
Even today, some clinicians claim they have “never met a DES daughter” whilst some women displayed many symptoms (ectopic pregnancies, late miscarriages, etc.) for years without having their condition correctly diagnosed. Researching and disseminating information about the history and effects of DES was largely left to the doctors and the unspecialized media who were willing to cover the issue. As a result, misdiagnosis and inappropriate care, sometimes iatrogenic, were—if not the rule—at least a very common experience for these women.
Useless sentinels or how to avoid publicizing DES knowledge
Three distinct mechanisms kept DES knowledge limited in the French case: the failure to build sound epidemiological cohorts, the lack of visibility of “dedicated” clinical structures, and finally the very weak dissemination of epidemiological and clinical knowledge.
Today, the absence of a tracked cohort of exposed population in France is striking. Indeed, to date, authorities have not even attempted to build a vaginal cancer registry. While the information campaign of 1992 supported by DES Action International was presented in France as a “screening” campaign, it did not lead to anything lasting, unlike in the Netherlands where large cohorts of exposed research subjects were built around the same time. Today, in France, the only ongoing research on DES is two small clinical surveillance follow-up studies that do not collect epidemiological data. Consequently, French doctors must rely on Dutch and American cohorts for information related to the effects of DES exposure on the third generation and psychological effects or cancer prevalence in mature women of the second generation. Moreover, the knowledge derived from all these cohorts remained relatively confined.
Indeed, the limited clinical knowledge that has been gathered to date remains in the hands of a small number of people. Info-DES, an association mainly composed of DES mothers, in the early 1990s worked with mobilized clinicians to build the first French forums offering information and clinical follow-up to affected patients. But these consultations have never been labeled as such by public authorities or even by lodging hospitals. As a result, DES patients generally must already know their status and proactively contact an association to obtain medical social or legal support.
The very few DES consultations that have taken place since the 1990s allowed for experimentation and adaptation techniques (such as relocation of a sole embryo in AMP, specific suture techniques to avoid late miscarriages, etc.) that were never publicized. Information flowed between associations and the limited number clinicians who saw first-hand the effects of DES, but the limited number of scientific publications published on the topic gained little interest. It was only intervention by the Réseau-DES, which followed up on Info-DES, that the circulation of knowledge was organized: in the late 1990s, this small association established a scientific advisory board that reviewed various controversial issues and mobilized official health agencies on specific topics. Réseau-DES was also responsible for the release of the first patient-focused brochure in 2008.
France’s policy concerning maternity leave for DES daughters illustrates ongoing problems plaguing the national response to DES. Drawing on long-documented medical studies showing that the best prevention of late miscarriages is full rest for pregnant women, Réseau-DES lobbied and advocated for maternity leave for DES daughters for more than fifteen years. Their efforts were unsuccessful until 2010, a time when most DES daughters were nearing the end of their reproductive lives. Moreover, in practice, doctors and social security administrators today still rarely know about this recently adopted policy. An invisibility mechanism is thus replicated from mother to daughter, and extended from the medical field to social life.
A singular history or how endocrine disruptors did
not transform DES
If DES is perpetually forgotten and neglected, it is in part because it initially appeared as a peculiar story. Health problems associated with DES have been for many years minimized as they were documented, rarely subjected to systematic collection, and rarely linked to broader public health issues such as drug pharmacovigilance or transgenerational exposure. This singularization work that has characterized the French response to DES began with those that bear the greatest public health concern and responsibility for launching alerts. Dr. Henry-Suchet’s research on very young French DES daughters showed changes in vaginal cellular structures that were not present in those exposed to ethinyl-estradiol. As a result, hormonal treatments in general were not questioned except in relation to this one drug. At the same moment when the first case of vaginal cancer appeared in 1975, French pharmacovigilance was founded on the basis of anti-poisoning centers and was therefore focused on short-term effects of substances, unlike the U.S. epidemiological model, which was able to trace long-term effects. In this context, when some DES effects were finally taken seriously in 1977, it remained the only drug known with long-term demonstrated effects.
Associative work went in the same direction: It was primarily focused on information related to providing clinical care for DES daughters until 2000. Debates about oral contraception or the controversy over hormone replacement therapy which received major attention worldwide had no echo in this little DES world. The creation of an association focused on parenting, Filles-DES, reinforced this trend: ovarian stimulation to get pregnant through AMP, for example, was not seen as problematic. It was only when another association, Hhorages, was created in 2002 that a shift in framing—from “DES drug” to “DES substance”—occurred. For the first time, DES was not seen as an isolated case, but was included among the various artificial hormones given to pregnant women and, therefore, to which their fetuses are exposed. Centered on the recognition of psychological effects of DES exposure, this association is run by parents whose DES-exposed progeny experienced serious psychological problems, often resulting in suicide. They blame all hormonal treatments, and thus attempt to expand the range of acknowledged deleterious effects in DES offspring to include other widely prescribed hormones. Hhorages collects data from its members and seek alliances, especially among toxicologists and endocrinologists specializing in environmental issues who often occupy the position of snipers within their own discipline. One of the most visible results of this collaboration is a co-authored article published in Fertility & Sterility in 2011 describing the increase of hypospadias, the defect of the urethra in males that involves an abnormally placed urinary meatus, a condition typically labeled an ED effect, among DES grandsons. Nevertheless, this transformation in the ED paradigm was not embraced by some French DES associations, which criticized that publication as “sensationalist.” At the heart of this debate lies the question of transmissibility: Did the nightmare stop with DES daughters or should exposure to the hormone be viewed as a real transgenerational threat for these daughters’ own progeny?